Chronic Obstructive Pulmonary Disease(COPD)
“Chronic obstructive pulmonary disease”(COPD)is a term for certain types of irreversible lung and airway damage that block(obstruct)your airways and make it hard to breathe.If you’re diagnosed with either emphysema or chronic bronchitis,you have COPD.
“Chronic obstructive pulmonary disease”(COPD)is a term for certain types of irreversible lung and airway damage that block(obstruct)your airways and make it hard to breathe.If you’re diagnosed with either emphysema or chronic bronchitis,you have COPD.
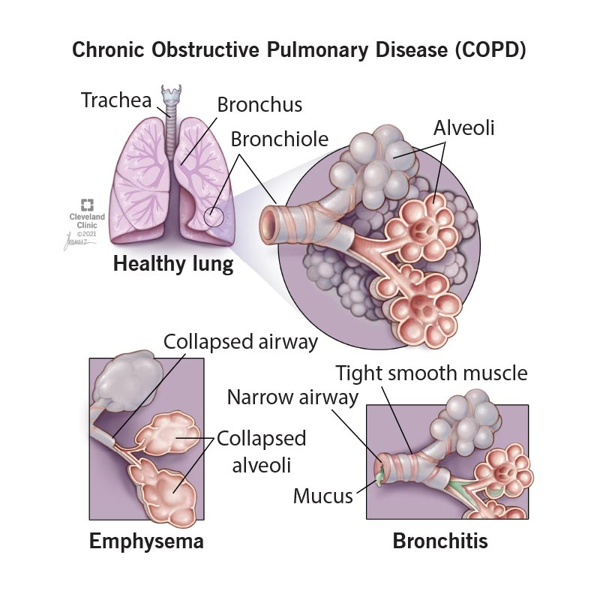
Changes in your lungs and airways in COPD include:
- Loss of elasticity in your airways and air sacs in your lungs(alveoli).
- Inflammation,scarring(fibrosis)and narrowing of your airways.
- Thick mucus in your airways.
- Destruction of the walls between your alveoli.This enlarges them and traps air.
People with COPD often get exacerbations,or worsening of symptoms,like severe difficulty breathing,thicker mucus,wheezing and cough.You might need to go to the hospital for severe exacerbations.
COPD gets progressively worse over time.Flare-ups get more severe and happen more often.This usually takes years or decades,though some people get worse faster.
Types Of Chronic Obstructive Pulmonary Disease
COPD includes both emphysema and chronic bronchitis.People with COPD often have features of both.
Emphysema is when your alveoli become damaged and enlarged.The most common symptom is shortness of breath(dyspnea).
Chronic bronchitis is inflammation in your large airways.This narrows your airways and makes lots of mucus.Cough is the most common symptom.
Symptoms And Causeswhat Are The Symptoms Of Copd?
Symptoms of COPD include:
- Cough with mucus that you’ve had for a long time(for three months or longer at a time for at least two years).
- Difficulty taking a deep breath.
- Shortness of breath,especially when performing daily activities or with mild exertion.
- Wheezing or otherlung sounds.
- Barrel-shaped chest.
- Bluish skin(cyanosis).
What Causes Copd?
Damage to your lungs fromsmokingis the most common cause of COPD.Other causes include:
- Alpha-1 antitrypsin deficiency(“alpha-1”),a genetic disorder that can lead to lung damage.
- Secondhand smoke.
- Air pollution.
- Exposure to dust and fumes from your job or hobbies.
What Are The Risk Factors For This Condition?
While smoking is the biggest risk factor for COPD,not everyone who smokes will develop it.You may be at higher risk for COPD if you:
- Are a personassigned female at birth.
- Are over the age of 65.
- Have been exposed to air pollution.
- Have worked with chemicals,dust or fumes.
- Have alpha-1 antitrypsin deficiency.
- Had many respiratory infections during childhood.
What Are The Complications Of Copd?
COPD can trapbacteriain your lungs,leading to infections.It can also prevent oxygen from getting into your body and carbon dioxide from getting out.This can lead to serious complications,including:
- Pneumonia.
- High levels of carbon dioxide in your blood(hypercapnia).
- Low levels of oxygen in your blood(hypoxemia).
- Respiratory failure.
- Pulmonary hypertension.
- Right-sided heart failure(cor pulmonale).
- Collapsed lung(pneumothorax).
- Polycythemia(making too many red blood cells).
Diagnosis And Tests
How Is Chronic Obstructive Pulmonary Disease(Copd)Diagnosed?
To diagnose COPD,a provider will performan examand ask you about your health history.They’ll test how well your lungs work and might get images of your lungs.
They may ask you questions like:
- Do you smoke or have you ever smoked?
- Have you had long-term exposure to dust or air pollutants?
- Do other members of your family have COPD,other lung conditions or liver disease?
- Do you get short of breath with exercise?When resting?
- Have you been coughing or wheezing for a long time?
- Do you cough up phlegm?
What Tests Do Healthcare Providers Use To Diagnose Copd?
Your provider might use the following tests to help diagnose COPD:
- Pulmonary function tests.Providers can usespirometry and other tests to see how well your lungs are working.
- Pulse oximetry.This test uses a device on your finger to measure oxygen levels in your blood.
- Imaging tests.Chest X-rays orCT scanscan look for lung changes caused by COPD.
- Arterial blood gas test.This is a blood test that checks your oxygen and carbon dioxide levels.
- Exercise testing.Your provider uses this to determine if the oxygen level in your blood drops when you exercise.
- Electrocardiogram(ECG or EKG).This test checks heart function and rules out heart disease as a cause of shortness of breath.
- Blood tests.Yourprovider may check your levels of the protein AAT to see if you might have Alpha-1 antitrypsin deficiency.
- Genetic testing.If your provider thinks a genetic condition could be causing your lung issues,they may check for genetic changes with a blood test.
What Are The Stages Of Copd?
Your provider can stage COPD based on your forced expiratory volume in one second(FEV1)results.FEV1 is the amount of air you can breathe out in one second,and it can tell your provider how blocked your airways are.Your provider measures FEV1 with spirometry.
COPD stages based on severity are:
- Stage 1:FEV1is 80 or above.
- Stage 2:FEV1is between 50 and 79.
- Stage 3:FEV1is between 30 and 49.
- Stage 4:FEV1is less than 30.
Your provider can also evaluate your symptoms and your risk for exacerbation using groupings with the letters A,B and E:
- A:You have mild symptoms and a low risk for exacerbations.
- B:You have more severe symptoms and a low risk for exacerbations.
- E:You have a high risk for exacerbations.
Your stage isn’t directly related to your symptoms—for instance,you could be in stage 3 or 4 but still have mild symptoms.Your provider can use your stage,symptoms and number of exacerbations to guide your treatment.
Management And Treatment
How Is Copd Treated?
There’s no cure for COPD.Treatment focuses on improving your symptoms and reducing and treating exacerbations.Your provider may recommend:
- Smoking cessation programs.Ifyou smoke,quitting can slow down the progression of COPD.
- Inhaled medications.Bronchodilatorsand steroids can reduce inflammation and open your airways.These might come in aninhaleror as a liquid you put in anebulizer.
- Oxygen therapy.You may need supplemental oxygen to improve your oxygen levels.
- Pulmonary rehabilitation.This is an exercise and education program that can strengthen your lungs and help you manage COPD.
- Corticosteroids.You might need a course of steroids to reduce inflammation during an exacerbation.
- Positive airway pressure.Your provider might have you use aBiPAP machineto help you breathe,especially during an exacerbation.
- Antibiotics.If you have frequent bacterial infections in your lungs,your provider may prescribe antibiotics to prevent infections and exacerbations.
- Lung volume reduction(LVR).If you have severe COPD and you’re a good candidate,your provider may suggestsurgeryoravalve procedurethat reduces the trapped air in your lungs.
- Clinical trials.Clinical trials are tests of new treatments to see if they’re safe and effective.Your provider might recommend one if a new treatment could be a good fit.
Prevention
Can Copd Be Prevented?
The best way to prevent COPD is to avoid smoking and exposure to secondhand smoke and other pollutants that can damage your lungs.
People with COPD are more likely to get respiratory infections,which can lead to pneumonia or cause severe exacerbations of your symptoms.You can reduce your risk of infections by:
- Getting all of your recommendedvaccinations,includingflu,pneumococcal pneumonia andCOVID-19.
- Washing your handsfrequently.
- Disinfecting surfaces.
- Wearing a mask around others if your provider recommends it.
- Avoiding crowded places,especially during cold and flu season and when cases of COVID are high.
Outlook/Prognosis
Can a Person With Copd Get Better?
The damage to your lungs from COPD is permanent and doesn’t get better.But there are ways to manage your symptoms for a long time,and sometimes even improve them.Following your healthcare provider’s recommendation and a pulmonary rehabilitation program can help improve your symptoms and your quality of life.
Can You Live a Long Life With Copd?
How long you live with COPD depends on how severe it is and how quickly it’s progressing.Many people can live for decades after diagnosis,especially with early treatment.People in stage 3 or 4 have a life expectancy that’ssix to nine years shorter than average.
Is Copd a Terminal Illness?
COPD gets progressively worse over time,but it’s not always a terminal illness.How quickly it progresses varies from person to person.Over time(usually years or even decades)many people with COPD won’t be able to breathe on their own.But others can live a long time without having severe symptoms.
Living With
How Do I Take Care Of Myself With Copd?
If you have COPD,some tips to take care of yourself include:
- Avoid lung irritants and anything that makes your symptoms worse.Thisincludes smoking,secondhand smoke,dust,air pollution and strong fragrances.
- Attend pulmonary rehabilitation sessions.This includesphysicalandoccupational therapyand education sessions.Keep up with the plan they outline even after your sessions have ended.
- Talk to a registered dietitian.They can tell you if there are specific foods to eat or avoid that can help keep you healthy.
- Take all of your medications as prescribed.Make sure you have daily medications on hand before you run out.
- Make a plan for flare-ups.Work with your provider on a plan for what to do if you have an exacerbation.This might include having certain medications on hand and knowing when to go to the hospital.
- Know how to use your medical devices.This can include inhalers,nebulizers,a CPAP machine and other devices.Ask your provider to demonstrate correct usage.
- Take care of your mental health.Having a chronic illness can take a toll on your mental health.A mental health provider like apsychiatrist,psychologistor counselor can help you manage social,emotional and other mental health issues.
When Should I See My Healthcare Provider?
If you think you could have COPD,don’t wait to see a healthcare provider.Early diagnosis and treatment can reduce your risk of your symptoms progressing.
If you have COPD,see your healthcare provider if you have signs of an infection or other changes in your symptoms,including:
- Worsening shortness of breath.You may notice that you can’t walk as far as you used to,you’re having more breathing difficulty at night,or you’re using your breathing treatments or inhalers more often than usual.
- Mucus(sputum)changes.This could include changes in color,bloody mucus,a foul smell,more mucus or thicker mucus than usual.
- Increased coughing or wheezing.
- New or worsening swelling in your ankles,feet or legs.Contact your provider if it doesn’t go away after a night’s sleep with your feet up.
- Unexplained weight lossor gain.
- Frequent morning headaches or dizziness.
- Unexplained,extreme fatigue or weakness.Contact your provider if it lasts for more than a day.
- Feveror chills.
- Other signs of infection.These could include sore throat,unusual sinus drainage,nasal congestion,headachesortenderness along your upper cheekbones.
When Should I Go To The Er?
Go to the emergency room if you experience:
- High fever(over 103 degrees Fahrenheit/40 degrees Celsius).
- Sudden or severe difficulty breathing.
- Restlessness,confusion,forgetfulness or irritability.
- Slurred speech.
What Questions Should I Ask My Healthcare Provider?
It might be helpful to ask your healthcare provider:
- What are the best ways to take care of myself?
- Can I improve my symptoms?
- How do I take this medication?
- How do I use my inhaler,nebulizer or other medical devices?
- When should I follow up with you?
- When should I go to the ER?
A Note From Cleveland Clinic
Living with chronic lung disease like COPD might feel overwhelming,scary,frustrating or even lonely at times.But there are ways to keep your lung muscles strong for as long as possible and even improve your symptoms.Making a plan with your healthcare team that will keep you healthy and reduce exacerbations can help it feel more manageable.Talk to your loved ones about how they can help,and what to do if you have a flare-up.
If you feel out of breath frequently,have a chronic cough or feel tired easily,don’t wait to talk to a healthcare provider.Early diagnosis can improve your quality of life and help keep you healthy for the years ahead.